Two-day training focuses on rural health-care scenarios
Realistic emergency scenarios, mixed with a little humour, have physicians, nurses, and paramedics sharing a new respect for one another’s roles following a course on rural health-care training.
The Comprehensive Approaches to Rural Emergencies (CARE) course was delivered to about 48 health-care providers in Brooks and Rocky Mountain House earlier this year. CARE, which was developed by British Columbia physicians, Rebecca Lindley and Jel Coward, brings doctors, nurses, paramedics, and other health-care workers together in an effort to promote teamwork.
Participants ranging from medical students to long-term health-care providers took part in the intensive two-day course, which features scenario training in medical, trauma and obstetric emergency management, with no testing at the end.
An eye opening experience

Everyone appreciated the humour woven throughout the sessions, and participants praised facilitators for their ability to keep everyone engaged despite the full days.
The Rural Health Professions Action Plan (RhPAP) funds four CARE courses annually throughout Alberta for communities with a population under 15,000.
Becky Brown has seen a lot of emergencies during her four-decade tenure as a registered nurse (RN) in Brooks. Seeing first-hand what the paramedics do before they arrive at the hospital really opened Brown’s eyes to the challenges they face in an uncontrolled environment.
“It’s always easy to see what was not done,” said Brown, noting she’ll now have a better grasp of why something like intravenous possibly wasn’t started before arriving at the hospital.
‘We didn’t sit at all’
During the pre-reading, LPN Jordan Watt was concerned the days would be filled with long lectures. “We didn’t sit at all,” she said. Instead, the 10-hour days were filled actively participating in applicable simulations and gave the Rocky Mountain House team an opportunity to bond.
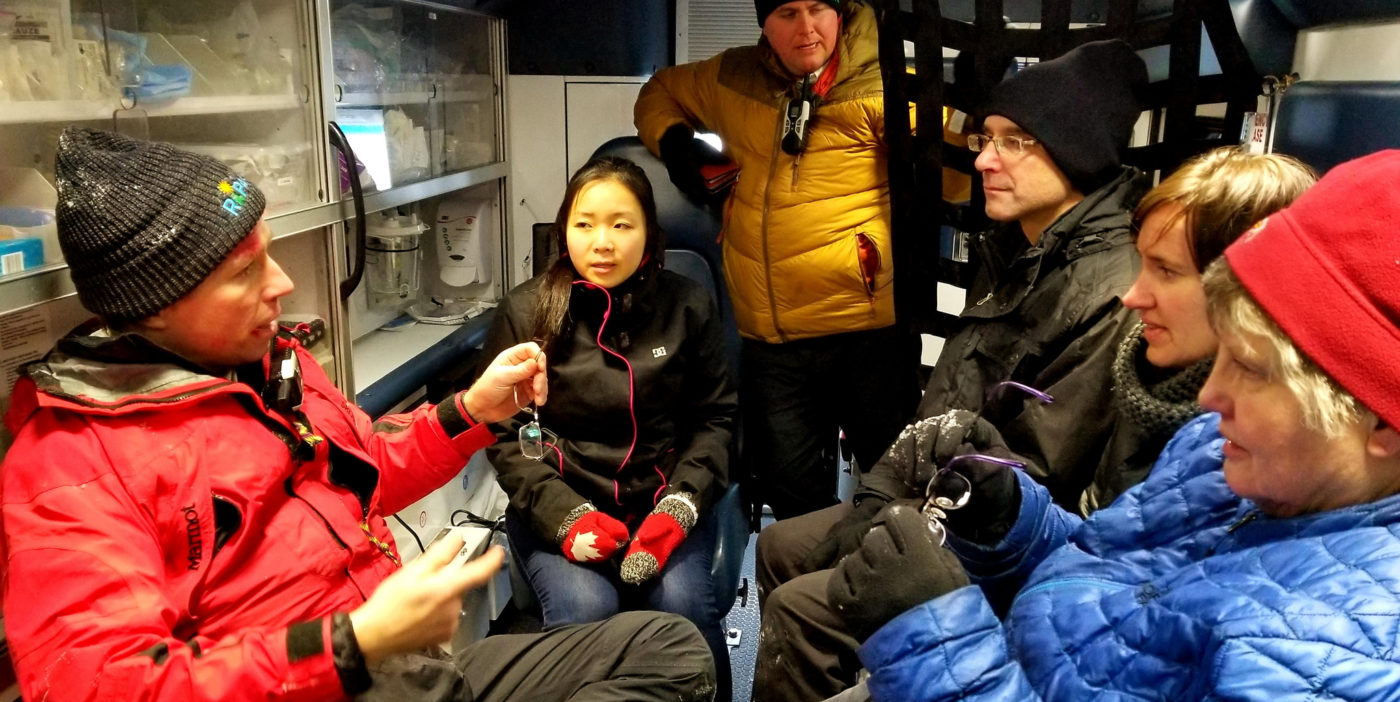
Dr. Dotun Ajibade, who has worked as physician in Brooks over the past year, recalled one aspect of the course where participants went outside in frigid temperatures to treat a patient.
“You are like, ‘whoa,’ in those scenarios as a doctor. You kind of feel helpless because this is not my comfort zone at all.”
While used to dealing with emergencies in the ER, Ajibade is typically backed by colleagues, tools, and equipment, and even security support if need be.
“Normally (paramedics) bring in the patients and you never see what they do out in the field,” he said. “I’m better able to understand the limitation of the paramedic … and I’m also able to see they are capable of a lot of things I probably didn’t give them credit for.”
Building relationships
Cody Frenette, a primary care paramedic based out of Nordegg, appreciated the opportunity to hone his skills while building relationships.
The course emphasized there are different ways to approach various emergencies and the discussions afterwards were always positive and non-judgmental.
“It was an amazing experience and well worth my time,” Frenette said. The course, and encouragement from other participants, has prompted him to pursue higher education in health care.
Everyone appreciated the humour woven throughout the sessions, and participants praised facilitators for their ability to keep everyone engaged despite the full days.
“(As a clinician) you want to do the right thing — give the right drugs and make the right decisions,” noted Ajibade. “The instructors made it a relaxing, low pressure atmosphere where you weren’t worried about saying something silly.”
A simulating experience

“We’re often taught by the physicians or (take) nursing courses. Seeing (physicians) vulnerable in the sense that they are learning new things too changed the team dynamic. Often they are the leader and you take their direction.”– Amanda Paradis, RN
One simulation where a male doctor played a pregnant woman (yes, that’s correct!) without prenatal care and, unknowingly carrying twins, was memorable.
“That was just so funny it was a highlight,” said Maggie Gamble, a licensed practical nurse (LPN) who works at the Brooks Health Centre.
Another powerful moment for Gamble was being able to use the cardiac defibrillator. “As an LPN, I am seldom ever able to touch it because it’s one of the things that is out of our scope. Regardless, everybody should know how to use it because there will come a time when you need to know more than you are able to do.”
Better equipped to deal with emergencies
Another takeaway many have now adapted into their routines is the 20-second review. The quick recap — called for by any member of the health-care team during treatment — ensures everyone knows what is going on at a particular interval, details what’s completed and what the plan is to come.
Third-year University of Calgary medical student, Rebecca Pham, said she’s more confident to deal with emergencies now even if she’s faced with limited resources.
“I haven’t been too involved in the more serious cases that come in. It was so good to see with this (Rocky Mountain House) group they were so well-oiled and knew what they were doing.”
Practising emergency situations involving children was very helpful, said paramedic Belle Clark. While fortunately rare, they do create higher stress for health-care professionals and the procedures can vary from that of an adult.
Learning on the same level
“It was a fantastic course and very well facilitated. We could see what each other’s strengths were … and fill in the gaps. The teamwork was a huge portion of what we learned from the course.” — Kim Rogers, MD
RN Amanda Paradis appreciated learning on the same level as other health-care providers such as physicians and paramedics.
“We’re often taught by the physicians or (take) nursing courses. Seeing (physicians) vulnerable in the sense that they are learning new things too changed the team dynamic. Often they are the leader and you take their direction.”
Rocky Mountain House physician, Kim Rogers, touted the benefits of hands-on experience with simulations on airway management, head injuries, paediatric, obstetric and cardiac cases.
“It was a fantastic course and very well facilitated. We could see what each other’s strengths were … and fill in the gaps. The teamwork was a huge portion of what we learned from the course.”
As Becky Brown discovered, the two-day training reinforced there is always more to learn.
“A lot of times, when courses are offered, you sign up hoping you are going to learn something,” Brown added. “I didn’t feel intimidated at all. In fact, it empowered me and that I had the knowledge. It actually gave everybody opportunities to shine.
“This was probably the best course I’ve had in my 44 years of nursing.”
- Article by Lorena Franchuk
