The World Health Organization proclaimed 2020 as Year of the Nurse and the Midwife—a tribute to the front-line caregivers in health care. The year was chosen to coincide with the 200th anniversary of English nursing pioneer Florence Nightingale’s birth to bring attention to this valued profession.
This week, Rural Health Beat steps back in time to learn more about Alberta’s early district nurses, who were often the only trained caregivers in isolated areas. Over the coming weeks, we’ll explore the present experience of rural registered and licensed practical nurses, nurse practitioners, midwives, and the other professionals who deliver care every day to rural Albertans – from newborns through to the elderly.
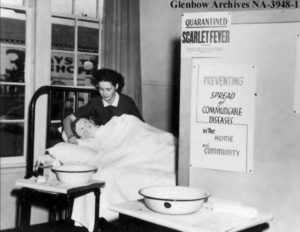
Remote areas received a spoon full of medicine and more from early district nurses
Single women looking for adventure helped bring health care to Alberta’s frontier in the early 20th Century.
District nurses met the challenge of providing much of the health care, particularly obstetrical care, in rural and remote Albertan communities. These women were often trained in Eastern Canada, the United States, and Britain, making practice in rural Alberta an adventure.
“[The use of District nurses] had been a long time coming as there was a lot of perceived feminist activism around women calling for access to … maternity services and basically saying that ‘you know, we’re the ones that are … doing the labour of populating the province by having babies. The province needs to support us in this,’” said Emily Kaliel, a University of Guelph PhD history student, who completed her master’s thesis on the development of Alberta’s district nursing program.
Kaliel’s interest in this nursing program derives from the experience of her grandparents, who welcomed district nurses into their circle in the Fawcett region, northwest of Whitecourt, in the 1940s and 1950s.
Alberta’s district nursing program was launched in 1919, when Alberta’s Department of Public Health borrowed some ideas from Manitoba to design their own program to meet Albertan needs. Public health nurses were already serving larger communities and sometimes undertook rotations to serve isolated areas. To qualify for a district nurse, communities had to be at least 60 km away from a railway station.
Washing newborn babies in frying pans and then wrapping them in my petticoat, at the time, seemed a natural thing to do, as did rushing to deliver a colt one night…” – Isabella Thyne, former district nurse for Lesser Slave Lake
“The biggest difference [between district and public health nurses] is that [the latter] never lived in a [remote] community,” Kaliel explained. “It was most often [district nurses who] were stationed in [a] northern or western region.”
District nursing was an intriguing concept for many women both fresh from training and those with experience from the First World War. District nursing allowed them to work without the supervision of a physician. Following the passing of the Public Health Nurses Act in 1919, district nurses were “given special dispensation to practise any of the services that a doctor could.” These services included the ability to practise midwifery, dispense medication, and make diagnoses.
“These nurses had so much leeway in terms of practice,” said Kaliel. “For some of them, that was a draw.”
District nurses were generally hired by the province or local districts to offer obstetrical, public health care (inoculations, proper hygiene, and education on accepted health-care practices), and emergency medical services such as dealing with appendicitis, a common ailment during that time. The health department, in most cases, paid them a salary averaging about $40 a month, she said.
French-speaking Alvine Cyr, a head nurse at the Edmonton General Hospital, was attracted to Plamondon, a community two hours northeast of Edmonton, after hearing a priest report on how many mothers were dying in childbirth.
“My mind was made up to go back with him before he had finished telling me the saddest stories I had ever heard of little children being left motherless,” Cyr recalled for the book, These Were Our Yesterdays: A History of District Nursing in Alberta compiled by Irene Stewart. She was a district nurse herself in Smith, midway between Athabasca and Slave Lake, in the 1930s.
Cyr’s posting in Plamondon ended up spanning two years.
“I was given $10 a month for the first two months only. Then I was able to collect fees, but the people were so poor that I accepted eggs, milk, and garden produce as payment,” Cyr explained.
Despite their daring nature, district nurses were often taken aback by the rugged conditions in places like Grande Prairie, Peace River, Slave Lake, and even farther north.
The biggest difference [between the district and public health nurses] is that [the latter] never lived in a [remote] community. It was most often [district nurses who] were stationed in [a] northern or western region.” Emily Kaliel, a University of Guelph PhD history student.
Scottish nurse, Isabella Thyne, was one of the fortunate ones who had experienced Northern Alberta as a child. As Stewart noted, Thyne returned to Alberta from Scotland as an adult with “fever” and maternity training, and immediately questioned her decision to come back.
“After my arrival in Edmonton [on] November 5, 1926, I was sent to Lesser Slave Lake,” Thyne recalled. “I got off the train at 3 a.m. in a terrible thunderstorm to see only one man in a horse-drawn wagon (who refused to move my trunk), a tiny shack (the station) and lots of mud. I asked the conductor when the train went back to Edmonton and was told ‘next week.’”
After a bumpy, muddy ride, Thyne arrived at a small white shack.
“As there was no bedding and no cooking utensils, I could not even make a cup of tea for warmth. I lay on top of the bed and realized that with the coming of morning, I would be tackling the biggest challenge of my life,” she said.

The next day, Thyne visited the forestry supervisor who brought her some much-needed supplies.
“I stayed with many lovely and hardworking people, who were very appreciative and helpful,” said Thyne. “Washing newborn babies in frying pans and then wrapping them in my petticoat, at the time, seemed a natural thing to do, as did rushing to deliver a colt one night … (He turned out to be a beauty, too).”
Horseback was Thyne’s main mode of transportation, but she also travelled by railway speeder [or handcar] to emergencies in Kinuso, Faust, and Smith, and often relied on a dog team during the winter to cover a roughly 325 square km territory.
Work for a district nurse was taxing, Kaliel explained
“What was asked of district nurses was just not possible. Their districts were huge, their transportation was very unreliable, infrastructure was also kind of non-existent, and they didn’t really have good communication technology … They very likely would not have been able to … physically survive if the community hadn’t really been on board with providing all those materials and services,” she added.
Many women had short stints as district nurses before they moved to other areas to nurse or left their careers behind to get married.
The introduction of travelling clinics helped relieve the pressure on district nurses, but their services came into great demand again with the outbreak of the Second World War. During the war, regions that could previously afford higher paid doctors often lost their physicians to the war efforts and relied on district nurses to fill this void.
Isolated communities continued to cherish the 24/7 care delivered by their beloved nurses into the 1950s.
“[District nurses] kind of just have this sweet spot, I think, in a lot of rural communities,” Kaliel said. “They were really revered by the communities that were lucky [enough] to have them.”
– Lorena Franchuk
