Saluting nurse practitioners during #NPWeek
RhPAP sends a shout out to all the nurse practitioners across rural Alberta during National Nurse Practitioner Week, which is taking place from November 13 to 19. Thank you for your dedication in keeping health care close to home for people throughout rural Alberta.
Rural nurse practitioner helps fill gap in local primary care access
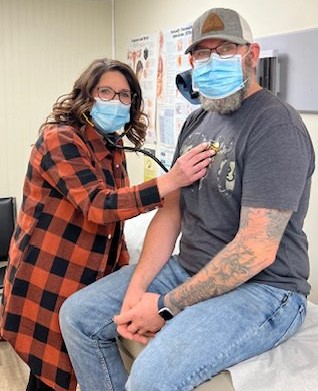
— Photo supplied by Michelle Williams
After working for two decades as a registered nurse based mainly in rural Alberta, Michelle Williams believed she could do even more for her patients.
“I had been an [registered nurse] for nearly 20 years and worked mainly in rural health care and hospital settings. I had done a specialty in palliative care and directed my practice more toward end of life care which I loved, but always thought, ‘I feel like I want to do more.” she explained.
Williams returned to school to become a family nurse practitioner (NP) while she worked simultaneously as a palliative care nurse consultant with Alberta Health Services. After graduating with a master’s degree in Nursing and completing her NP clinical components, she realized her true calling was helping rural Albertans.
With her new NP designation, Williams was able to put her medical experience and training towards that of a primary care provider.
“With a nursing background, [nurse practitioners are] trained to look at the whole person and provide true patient-centered care,” she said.
“We do routine health screening such as PAP tests, physical exams, and manage chronic conditions. We can order labs and X-rays and interpret the results. We prescribe medications including narcotics and do procedures such as skin biopsies, IUD [intrauterine device] insertions, and suturing. We are able to make referrals to specialist physicians as well as perform driver’s medicals, WCB assessments, and complete disability forms.” she said.
An opportunity for an NP position opened up with the Leduc Devon Beaumont Primary Care Network (PCN) in December 2019 through a grant under the province’s Nurse Practitioners Support Program.
Williams would be able to provide primary care to residents in the western region of Leduc County based clinics in Thorsby and Warburg. Prior to her arrival, patients would travel to Calmar, Devon, Leduc or Drayton Valley to see a physician—which wasn’t always feasible due to distance and other reasons.
Even if patients could travel, many physicians weren’t accepting new patients.
“People had been [limited in options] so they were just ignoring their health,” she said of the catchment area of about 10,000 people with a high population of seniors.
Williams jumped at the opportunity to play a key role in her patients’ health and wellness.
Williams, under the PCN, worked with various community stakeholders including the municipalities of Warburg and Thorsby, Leduc County, and Alberta Health Services so the clinics could open.
“When I was hired and started working in January of 2020, my efforts were focused on developing the clinics from the ground up with all the technical components of establishing a medical clinic including securing clinic space in both communities,” she said of the work which also included IT setup and ordering equipment.
“It’s a true success story in terms of stakeholder collaboration, innovation, and dedication towards the common goal of improving access to primary healthcare” — Michelle Williams.
Williams admitted it was a steep learning curve for a new NP, especially without clinic management expertise. Fortunately, the stakeholders were able to provide some funding to hire a medical office assistant who had experience working in a clinic.
“It’s a true success story in terms of stakeholder collaboration, innovation, and dedication towards the common goal of improving access to primary healthcare, said Williams.
“I hope that we can use this as a model for other rural communities to exemplify that advocacy and team work can truly make things happen.”
Dr. Susan Prendergast, president of the Nurse Practitioner Association of Alberta, and a former midwife and RN who now works as a nurse practitioner, says the NPAA and national counterparts have worked for years to encourage interested RNs already living rural to continue their education and become NPs possibly with rural specialization.
“The challenge [for a] rural NP actually is that if you haven’t worked in a rural area before, it might be a little bit more work to try to become embedded in the community,” said Dr. Prendergast.
“So what we’ve been doing nationally is trying to plan for that sort of preparation for nurse practitioners.”
Dr. Prendergast said in addition to the many who have already been fully trained as NPs, a number of RNs are interested in pursuing further education to expand their scope of practice.
Williams said it’s her patient satisfaction that keeps her going strong as a full-time NP on call 24/7.
Past studies on NP care mirror that perception.
“We’ve done a lot of evaluation work and the satisfaction rate from patients is very high,” said Williams. “Nearly 100 per cent of patients surveyed said that they were very or 100 per cent fully satisfied with the care they’ve received.”
Both Williams and Dr. Prendergast maintain there is plenty of work and collaboration opportunities for physicians and NPs to provide primary health care for rural Alberta and elsewhere.
“There’s room for everybody. If you could get a physician and a nurse practitioner, it’s a wonderful mix.” said Dr. Prendergast.
“You bring different things to the table.”
— Lorena Franchuk
